When Should You Be Concerned About Suddenly Appearing Veins?
Understanding the Causes, Risks, and When to Seek Medical Help
Suddenly visible or protruding veins on your body can be surprising, and even alarming. While in many cases they may be completely harmless—often related to physical exertion, aging, or temperature changes—there are times when newly prominent veins may signal an underlying health issue that requires medical attention.
This article explores the possible causes of suddenly visible veins, how to distinguish harmless from concerning changes, and when you should seek professional evaluation.
What Causes Veins to Suddenly Appear?
Veins become more visible for several natural or temporary reasons, including:
1. Physical Activity
During or after exercise, blood flow increases and muscles push veins closer to the surface of the skin. This can make veins appear larger, especially in areas like the arms, hands, and legs. This is known as “vascularity,” and it’s common among athletes and bodybuilders.
2. Aging
As we age, skin loses collagen and becomes thinner. This makes veins more visible, especially on the hands and arms. Additionally, venous valves can weaken with age, sometimes causing bulging veins.
3. Temperature Changes
Hot weather or showers can cause veins to dilate (expand) temporarily, making them more noticeable. Cold can have the opposite effect, causing them to contract.
4. Weight Loss
Losing fat—particularly subcutaneous fat (the layer under the skin)—can cause veins to become more prominent. This is common among people who lose weight quickly or reach very low body fat percentages.
5. Hormonal Changes
Hormones can influence blood volume and vascular tone. For example, during pregnancy or menopause, changes in estrogen and progesterone levels may make veins more visible or lead to spider veins or varicose veins.
When to Be Concerned: Warning Signs
While the above causes are generally benign, certain symptoms and sudden changes in vein appearance may be red flags for underlying health problems.
1. Swelling or Pain
If your visible veins are accompanied by swelling, tenderness, or a warm sensation, this could be a sign of deep vein thrombosis (DVT)—a serious condition where a blood clot forms in a deep vein, often in the leg. DVT can lead to life-threatening complications like pulmonary embolism.
2. Color Changes
Veins that appear red, purple, or dark blue, especially if they’re painful or inflamed, could indicate phlebitis (vein inflammation) or infection.
3. Sudden Appearance in One Limb
If veins appear suddenly and prominently in just one leg or arm, and are associated with discomfort, it may point to a circulatory blockage or vascular disease.
4. Accompanied by Skin Changes
If veins appear with ulcers, flaky skin, discoloration, or itching, this may suggest chronic venous insufficiency, where blood pools in the legs due to valve failure in the veins. This condition can worsen over time and requires medical management.
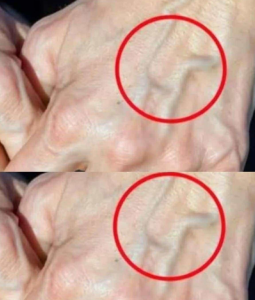
5. Bulging and Rope-Like Appearance
Varicose veins, which appear swollen, twisted, and raised, can become problematic if they cause discomfort, fatigue, or lead to ulcers. They result from faulty valves and are more than a cosmetic issue when they impair daily function.
6. Rapid Onset Without Clear Cause
If veins appear suddenly and without an obvious reason like exercise, weight loss, or heat exposure, especially if you’re not prone to vascular visibility, this warrants attention. Sudden vascular changes can sometimes be linked to autoimmune conditions, vascular tumors, or blood flow abnormalities.
Underlying Conditions That Can Cause Prominent Veins
If suddenly visible veins aren’t related to lifestyle factors, some possible medical conditions include:
1. Deep Vein Thrombosis (DVT)
A clot in a deep vein that blocks circulation. Symptoms include pain, swelling, heat, and sometimes visible surface veins due to rerouted blood flow.
2. Chronic Venous Insufficiency (CVI)
This occurs when vein valves fail to close properly, allowing blood to pool. Over time, veins become more prominent, and symptoms may include aching, heaviness, or skin discoloration.
3. Superior Vena Cava Syndrome
A rare condition where the superior vena cava (a large vein returning blood to the heart) is partially blocked, often due to tumors or infections. This can cause swelling in the face, neck, and arms with visibly engorged veins.
4. Liver Disease (e.g., Cirrhosis)
Cirrhosis can cause spider veins or caput medusae (veins radiating from the abdomen) due to increased pressure in the portal vein (portal hypertension).
5. Autoimmune or Connective Tissue Disorders
Diseases like scleroderma or vasculitis can affect blood vessels and make them more visible or inflamed.
6. Blood Clotting Disorders
Conditions that increase clot risk—such as Factor V Leiden mutation or antiphospholipid syndrome—can result in clots that affect venous appearance.
When to See a Doctor
You should consult a healthcare professional if you experience:
-
Sudden vein visibility with no clear cause
-
Pain, tenderness, or swelling near the vein
-
Color or texture changes in the skin
-
Bulging, twisted, or rope-like veins
-
Persistent leg fatigue, heaviness, or itching
-
Ulcers or sores around the ankles or legs
-
Shortness of breath or chest pain (seek emergency care, could indicate a clot has traveled to the lungs)
Diagnosis and Tests
If you present with concerning vein symptoms, a doctor may order tests such as:
-
Duplex ultrasound to check for blood clots or valve issues
-
Venography, an X-ray with contrast dye to view veins
-
Blood tests to check for clotting disorders
-
CT or MRI scans if deeper vascular structures are suspected to be involved
Treatment Options
Treatment depends on the underlying cause. Some common approaches include:
-
Compression stockings to improve circulation in chronic venous insufficiency
-
Anticoagulants (blood thinners) if a clot is found
-
Sclerotherapy or laser therapy for varicose or spider veins
-
Lifestyle changes: regular exercise, elevating legs, avoiding long periods of standing or sitting
-
Surgery or vein ablation in severe cases
Prevention Tips
-
Stay active: Regular walking improves leg circulation.
-
Avoid prolonged sitting/standing: Move around every hour.
-
Maintain a healthy weight: Reduces pressure on veins.
-
Elevate legs: Especially after long days.
-
Stay hydrated: Keeps blood viscosity lower.
-
Wear compression socks: Especially for travel or jobs with long standing hours.
Final Thoughts
Suddenly visible veins aren’t always a cause for panic. In many cases, they’re related to lifestyle, genetics, or aging. However, if they appear without explanation, cause discomfort, or show warning signs like swelling, pain, or skin changes, they could indicate something more serious.
Your veins tell a story about your circulation, and when they change suddenly, it’s your body’s way of speaking up. Listening to it—early—can make all the difference.